"Changing Your Stress To The Best Quality of Life"
OSCE WORKSTATIONS
The OSCE is designed as a comprehensive evaluation tool, comprising 10 strategically crafted stations that collectively assess a candidate’s clinical competence and professional attributes.
APIE STATION
Four stations work together around a single clinical scenario, following the APIE framework Assessment, Planning, Implementation, and Evaluation. This integrated approach challenges candidates to apply a systematic method to clinical problem-solving, ensuring that every step of patient care is thoroughly examined.
Station 1: Assessment
In this station, candidates are tasked with conducting an in-depth, patient-centered evaluation to identify the patient’s specific nursing needs through the lens of their daily living activities. Using the Activities of Daily Living (ADL) model as your framework, you are expected to:
Record and Plot Vital Signs Accurately:
Ensure you perform a precise measurement and plotting of vital signs, establishing a dependable clinical baseline as part of your patient evaluation.Execute a Systematic A-to-E Assessment:
Carry out a structured assessment following the A-to-E approach (Airway, Breathing, Circulation, Disability, Exposure). This methodical process will help you identify any critical concerns quickly and comprehensively.
All of these tasks must be completed efficiently within the allocated 20-minute timeframe, demonstrating both your clinical competence and your ability to manage time effectively while providing high-quality patient care.
Guidelines:
Embrace a holistic approach
Practice active and empathic listening to the patient’s problems and concerns


Station 2: Planning
In this station, you are required to identify and document two key aspects of nursing care directly derived from the assessment in Station 1. You have 14 minutes to articulate these interventions precisely.
Guidelines for Effective Planning:
Focus on Relevance and Evidence:
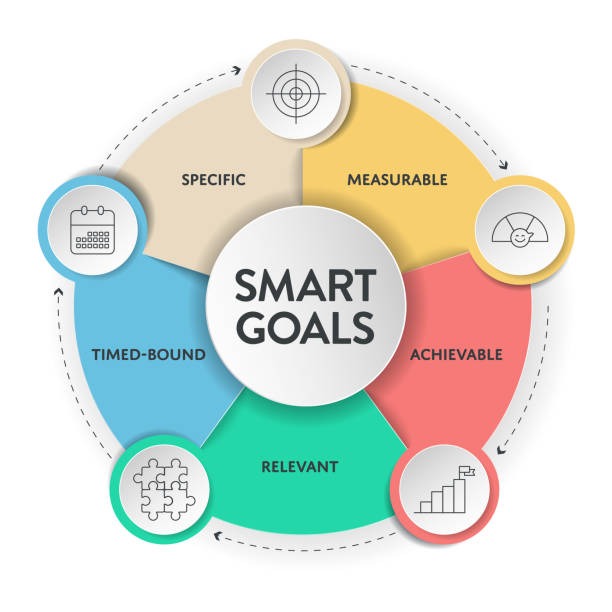
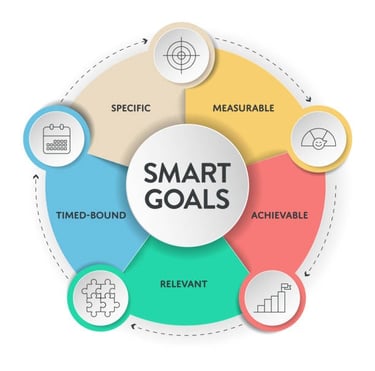
Select only the most pertinent nursing interventions that address the critical needs identified during your assessment. Ensure that each intervention is supported by current evidence and aligns with best practices in patient care.Utilize the SMART Framework:
Structure each intervention so that it is Specific, Measurable, Achievable, Realistic, and Time-bound. This approach will help you create clear, actionable, and goal-oriented care plans.Prioritize the Patient's Key Needs:
Concentrate on the two most important aspects of nursing care as determined by your assessment. Avoid including extraneous details—your focus should be on delivering high-priority interventions that yield meaningful outcomes.


Station 3: Implementation
In this station, you are required to demonstrate your ability to safely and accurately administer oral medications within a 15-minute timeframe. Your task is to follow established drug administration protocols and adhere to NMC guidance, ensuring optimal patient safety and care quality.
Key Objectives:
Precise Oral Drug Administration:
Administer the prescribed oral medications by following the correct principles. This includes verifying the right patient, drug, dosage, route, and time—ensuring that every administration step aligns with NMC standards.Adherence to NMC Guidance:
Ensure that every aspect of your practice from the preparation, administration to post-administration documentation fully complies with the latest NMC guidelines, reflecting the highest level of patient-centered care.
Guidelines:
Strategic Review of the Medication Administration Record:
Develop and implement a systematic method for reading and interpreting the medication administration record. Verify all details carefully and cross-check medication particulars to prevent errors.Meticulous Documentation:
Complete all required documentation thoroughly and accurately. Record the administration time, the exact dosage given, and any observations or patient feedback.


Station 4: Evaluation
In this station, you are expected to deliver a clear, concise, and systematic verbal handover of your patient within an 8-minute timeframe. Your handover should be structured using the SBAR framework:
Situation: Clearly state the current condition of the patient.
Background: Provide key contextual details, including relevant history and recent observations.
Assessment: Share your clinical evaluation and any immediate concerns.
Recommendation: Offer actionable suggestions for further care or management.
Guidelines:
Be Systematic:
Approach your handover methodically by following the SBAR format to ensure coherence and completeness.Prepare Written Notes:
Spend a few minutes before your handover to jot down clear, concise notes. These will serve as a reference to keep your information organized and ensure no critical details are missed.
SKILLS STATION
In these stations, you’ll be assessed on your ability to accurately and confidently demonstrate two paired clinical skills selected from a list provided by the test centre. Each skill is assigned its own dedicated time slot—Stations 5 & 6 form one pair, and Stations 7 & 8 comprise the second—so manage your time accordingly to complete each skill to a high standard.
Key Requirements:
Skill Pairing:
You should be well-prepared with the specific skills allocated by your test centre. Each pair will test your competency in executing two interrelated clinical procedures.Time Management:
Be mindful of the distinct time limits for each skill. Use your time strategically to ensure every step of the procedure is demonstrated thoroughly and competently.
Guidelines:
Listen to the Briefing:
Carefully pay attention to the examiner’s briefing at the start of each station. Listening attentively ensures you understand precisely which skill or combination of skills you need to demonstrate.Correct Use of PPE:
Always adhere to the proper use of Personal Protective Equipment (PPE) from start to finish. Demonstrating proper PPE usage is crucial for maintaining safety and compliance with clinical standards.Infection Control Practices:
Follow correct infection control protocols meticulously. This includes the proper handling and disposal of any clinical waste throughout the demonstration, ensuring that each step meets current health and safety guidelines.
This structured approach not only enables you to showcase your technical proficiency but also highlights your commitment to safety and best practices in clinical care.




SILENT STATION
The silent station challenges candidates to independently complete clinical tasks without any verbal communication or immediate feedback, simulating the high-pressure, real-world environments nurses often face. In this station, candidates are provided with written instructions or a patient case scenario, and must either develop a care plan or demonstrate essential clinical skills.
This exercise focuses on critical areas such as clinical decision-making, patient assessment, diagnostic interpretation, charting and documentation, and medication calculations and administration. The absence of interaction and feedback is intended to mirror situations like night shifts or emergency responses where quick, independent, and assured decision-making is crucial.
Consequently, mental preparation and resilience are fundamental, as the silence can amplify anxiety and uncertainty while rigorously testing the candidate's ability to interpret information, prioritize care, and act decisively under pressure.
Station 9: Professional Values
In this station, you'll be evaluated on your ability to express, through concise bullet points, the actions you would take in response to a given scenario. This exercise is designed to test your understanding and application of the NMC Code of Conduct as well as your commitment to core professional values.
Your Task:
After reading the scenario, respond by outlining your actions in clear, structured bullet points.
You have 10 minutes to complete this task.
Key Points to Cover:
Link to the NMC Code: Ensure your responses reflect the principles of the NMC Code, such as prioritizing patient care, maintaining professional integrity, and respecting the dignity and rights of all patients.
Demonstration of Professional Values: Your bullet points should highlight actions that embody your commitment to ethical practice, accountability, and empathy in every situation.
Top Tips for Success:
Carefully Read the Scenario: Take time to fully understand the context and its implications for professional practice.
Articulate Clearly: Write your bullet points in simple, straightforward language that clearly communicates your intended actions.
Structure Your Response: Organize your bullet points logically so that each step flows naturally into the next.
Be Familiar with the Marking Criteria: Understand what the test centres are looking for, so your response aligns with their expectations regarding clarity, relevance, and thoroughness.
Time Management: Keep an eye on the clock to ensure you complete your answer within the 10-minute time frame, covering all critical points.
This station is not just about what you know, but also how effectively you can apply that knowledge in real-world situations while upholding the professional values that are vital to quality patient care.
Top Tips:
Ensure Every Action is Evidence-Driven: Base each bullet point on reliable sources such as established research findings or recognized clinical guidelines.
Maintain Clarity and Precision: Write in simple, well-organized bullet points so that your rationale is easy to follow.
Know the Marking Criteria: Familiarize yourself with the specific requirements for Evidence-Based Practice scenarios as set by the test centre, to ensure your answer meets the expected standards.
Manage Your Time: With only 10 minutes allocated, prioritize your key points to cover all critical aspects of the scenario effectively.
By following these strategies, you will demonstrate not only your solid understanding of evidence-based practice but also your ability to make informed, reliable clinical decisions swiftly and under pressure.
Station 10: Evidence-Based Practice
In this station, you are required to assess a given scenario and a summary article, then articulate your actions in a series of clear, concise bullet points—all within a 10-minute timeframe. This task is designed to evaluate your application of evidence-based practice by ensuring that every decision and action you describe is grounded in high-quality research, clinical guidelines, or empirical data. You must demonstrate how you integrate sound evidence into your clinical decision-making process and align your care strategies with current best practices.
Mantebre Care
"Changing your stress to the best quality of life"
Contact
info@mantebre.co.uk
+44 07512143937
© 2024. All rights reserved.
Disclaimer
At Mantebre Company Ltd, we uphold a transparent and fair hiring process.
We do not charge any application or recruitment fees.
We do not work with agents or third parties for recruitment.
If you are ever asked to make a payment or engage with an intermediary claiming to represent us, please consider it a scam and report it immediately.
Apply directly through our official channels.
Focus on your qualifications — not payments.
We are committed to equal opportunities and a recruitment process built on integrity and trust.